Understanding Melasma
Melasma is a common yet complex pigmentation condition that causes dark, irregular patches on the skin, most often appearing on the face — cheeks, forehead, upper lip, and nose. While many people think of melasma as simply “skin discoloration,” it is far more intricate than that. It is a multifactorial skin condition involving not only excess melanin on the skin’s surface but also deeper changes within skin cells, inflammation, and the natural effects of ageing.
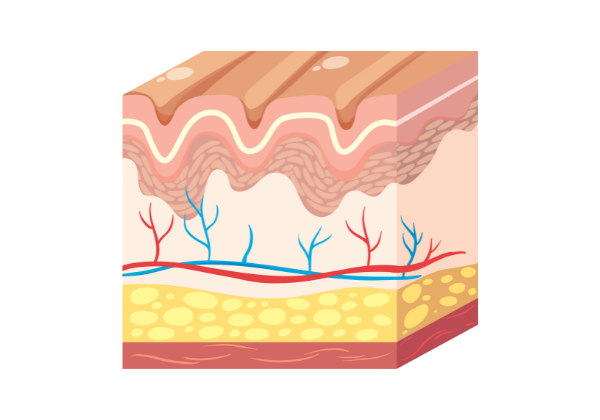
How Melasma Develops Under Your Skin
At its core, melasma develops from overactive melanocytes — the specialised skin cells that produce melanin, the pigment responsible for our skin colour. In melasma, these melanocytes become hypersensitive and overactive, leading to uneven melanin production and irregular dark patches on the skin.
Why Melasma is So Hard to Treat
Unlike typical sunspots or freckles, melasma is stubborn, recurrent, and deeply rooted. The pigment often extends beyond the epidermis into the dermis, making it harder to fade.
On top of that, melanocytes in melasma remain highly reactive, so even minor triggers — like sunlight, heat, or hormonal fluctuations—can reactivate pigmentation. This explains why many people notice initial improvement with treatment, only to see patches return.
Because of this complexity, effective management requires more than just surface-level treatments — it needs strategies that address both the visible pigmentation and the root cellular changes driving it.
Melasma Causes: The Hidden Triggers
Many people assume that melasma is only caused by sun exposure. In reality, it is a multifactorial condition that develops and persists due to a combination of underlying skin changes, environmental triggers, hormonal activity and genetic predisposition.
Underlying skin changes
The structure and function of the skin itself play a central role in how melasma forms and why it can be so persistent. When the skin barrier is compromised or when melanocytes become overactive, pigmentation tends to deepen and linger.
Key contributors include:
Aging and Slower Cell Turnover: With age, melanocytes—the pigment-producing cells—become more reactive, while the skin’s renewal cycle slows. This means melanin remains in the skin longer, leading to stubborn dark patches.
Weakened Skin Barrier: A compromised barrier allows irritants and pollutants to penetrate more easily, which causes inflammation and stimulates melanocytes.
Increased Vascular Activity: Higher blood flow and vessel activity in certain areas can intensify pigmentation, giving melasma its reddish-brown hue.
Irritation and Trauma: Harsh scrubbing, aggressive chemical peels, or skin injuries can worsen melasma by activating melanocytes in deeper skin layers.
Sunlight & environment
Among external triggers, sunlight is the strongest and most consistent cause of melasma. In a tropical climate like Singapore, where UV exposure, heat, and pollution are constant, environmental factors make melasma particularly common and difficult to manage.
Key contributors include:
UV Radiation: Both UVA and UVB rays penetrate the skin and directly stimulate melanocytes, darkening existing pigmentation and triggering new spots. Repeated exposure makes melasma more resistant to treatment.
Visible light (HEV): High-energy visible light from the sun and even digital devices can worsen pigmentation, especially in medium to darker skin tones.
Infrared Radiation and Heat: Infrared rays raise skin temperature, increasing vascular activity and oxidative stress. Heat also fuels inflammation, which contributes to deeper, more stubborn pigmentation.
Environmental Pollutants: Air pollution, dust, and toxins trigger oxidative stress, damage skin cells, and worsen melasma by further activating pigment-producing cells.
Hormones & Genetics
Hormonal activity and inherited traits are major internal drivers of melasma. This explains why the condition often appears during life stages or circumstances involving hormone fluctuations, and why some individuals are naturally more predisposed.
Key contributors include:
Pregnancy: Increased estrogen and progesterone stimulate melanocytes, giving rise to the “mask of pregnancy” that affects many expectant mothers.
Oral Contraceptives and Hormone Therapy: Birth control pills or hormone replacement therapy can overstimulate melanocytes in individuals already prone to pigmentation.
Menopause and Hormonal Fluctuations: Shifting estrogen and progesterone levels during perimenopause and menopause can increase skin’s vulnerability to melasma.
Genetic Predisposition: People with medium to darker skin tones (Fitzpatrick III–V) and those with a family history of pigmentation are more susceptible, as their melanocytes are inherently more reactive to triggers.
Our Multi-Layered Approach to Treating Melasma
Because melasma has multiple triggers and its highly individual, we don’t rely on a single treatment. Instead, our doctors prefer a combination strategy, tailored to each patient’s skin type, triggers, and melasma depth. This approach targets both stubborn surface pigmentation and the overactive melanocytes beneath, giving patients the best chance for lasting, transformative results.
Laser Treatments
Lasers remain a cornerstone in managing melasma, but their success depends entirely on precision, medical supervision, and carefully calibrated protocols.
At our clinic, we employ a range of systems — including Picosecond Lasers, Q-switched Lasers, and the Multifrax Digital Peel — tailoring wavelength, energy, and treatment intervals to each patient’s unique skin type and melasma depth.
This customised approach prevents overheating (a common cause of rebound pigmentation) while ensuring that excess melanin is broken down into microscopic particles. These are then gradually cleared by the skin’s repair mechanisms.
When delivered in a protocol-driven, doctor-led manner, laser therapy not only lightens stubborn pigmentation but also refines skin clarity, smoothness, and overall resilience.
Benefits:
Breaks down excess melanin for clearer, more even skin tone
Improves skin clarity and texture with minimal downtime
Uses multiple protoccols tailored to melasma’s depth and type
gold rf microneedling
Gold RF Microneedling is the world’s first dual-wave microneedling system that delivers controlled radiofrequency energy through ultra-fine, gold-coated microneedles into the skin’s deeper layers.
This procedure directly addresses the vascular, inflammatory, and pigment-related pathways that drive melasma, while simultaneously stimulating collagen and rebuilding the dermal support matrix.
By calming overactive melanocytes and strengthening the skin’s defence against external triggers, it works at the root level of melasma rather than only fading surface pigmentation. This deeper correction not only reduces the likelihood of recurrence but also enhances the overall resilience of the skin.
As an added benefit, Gold RF Microneedling also improves skin texture, firmness, and clarity, making it a versatile treatment that contributes to both melasma control and broader skin rejuvenation.
Benefits:
Regulates melanocyte activity to reduce recurrent pigmentation
Stimulates collagen and repairs vascular factors linked to melasma
Strengthens skin structure, making it less reactive to triggers
Depigment Chemical Peel
For widespread melasma, our doctors may recommend a professional depigmenting system such as Cosmelan® or Dermamelan®. These chemical peels are formulated with medical-grade actives that reset overactive melanocytes and progressively reduce uneven pigmentation.
While these treatments also visibly reduce spots like a peel, they go further by regulating melanocyte activity and correcting excessive pigment production, targeting the root cause of melasma. By addressing the origin of pigmentation rather than only the surface, these methods help prevent recurrence while gradually restoring a more even, radiant skin tone.
When integrated into a comprehensive treatment program, depigmenting chemical peels work synergistically with lasers and RF microneedling to help accelerate pigmentation fading and support long-term control of melasma.
Benefits:
Resets overactive melanocytes for more even pigmentation
Smooths texture and refines skin tone over repeated sessions
Works synergistically with other melasma treatments for stronger outcomes
Infusion of clinical serums
Topical skincare alone often cannot penetrate deeply enough to influence melasma. That is why we use Lorient Element (a topical skinbooster) to deliver potent brightening serums directly into the skin using LDM Ultrasound.
These formulations go beyond cosmetic products — they are carefully selected to neutralise oxidative stress, calm overactive melanocytes, and restore the skin barrier. When combined with lasers or microneedling, these infusions reach target layers more effectively, improving overall melasma treatment results.
Benefits:
Delivers pigment-correcting actives deep into the skin
Neutralises inflammation and oxidative stress at a cellular level
Restores a healthier skin barrier to support lasting results
Prescription Skincare & Oral Support
Long-term melasma control relies on what happens beyond the clinic. Our customised skincare protocols include broad-spectrum sun protection, antioxidants, pigment-correcting actives, retinoids, and barrier-strengthening formulations to protect against daily triggers.
In selected cases, our doctors may recommend oral supplements such as Heliocare®, Crystal Tomato® or MitoQ Derma Elite® to create a protective environment for the skin, enhancing treatment outcomes and minimising relapse.
Benefits:
Protects skin daily with sunscreen, antioxidants, and retinoids
Enhances clinic results with oral nutraceuticals and supplements
Builds long-term skin health to minimise relapse and flare-ups
Frequently Asked Questions
-
Melasma rarely resolves completely without intervention, especially in adults. While minor pigment changes may fade over time, most cases are chronic and recurrent, particularly if triggers like UV exposure or hormonal fluctuations persist. Effective treatment often requires a multi-layered approach, including professional procedures, prescription skincare, and lifestyle modifications, to achieve sustained results.
-
No. While all involve pigmentation, melasma differs from sun spots or freckles in several ways. Melasma is usually larger, symmetrical, and more persistent, with pigment often located in both the epidermis and dermis, making it harder to treat.
Sun spots and freckles are typically surface-level, lighter, and more responsive to topical treatments, whereas melasma often requires multi-modality professional intervention for long-term control.
-
Choosing the most effective melasma treatment depends on several factors, including your melasma type (epidermal, dermal, or mixed), skin type, severity, triggers, and any previous treatments. Because melasma is complex and highly individual, it is best to consult a professional clinic, where a doctor can perform a thorough assessment using clinical evaluation and your personal history.
From there, a customized, multi-layered treatment plan can be designed, potentially combining lasers, gold RF microneedling, chemical peels, medical serums, prescription skincare, and oral supplements.
This ensures that both surface pigmentation and deeper melanocyte activity are addressed safely and effectively, giving you the best chance for long-lasting, stable results.
-
The timeline varies depending on the type, depth, and severity of melasma. Epidermal melasma may respond within 4–6 weeks of consistent treatment, while dermal or mixed melasma may take several months to show significant improvement. Multi-layered approaches combining lasers, microneedling, chemical peels, and prescription skincare typically yield the fastest and most durable results. Regular follow-ups are crucial to monitor progress and prevent rebound pigmentation.
-
Preventing recurrence requires consistent protection and maintenance, not just one-off treatments. Daily use of broad-spectrum sunscreen, sun-protective clothing, and minimizing heat and visible light exposure is critical. Supporting the skin barrier with medical-grade skincare, antioxidants, and pigment-correcting products also helps reduce triggers.
A comprehensive, ongoing plan tailored by a specialist is the most effective way to maintain results and keep pigmentation at bay.
-
Melasma often worsens in sunny and tropical climates like Singapore due to high levels of ultraviolet (UV) radiation, visible light, and heat, all of which stimulate melanocytes to produce more pigment. Even incidental sun exposure, such as walking outdoors or commuting, can trigger darkening of existing patches or the formation of new ones. This can be frustrating for patients who feel their pigmentation returns despite treatments.
Understanding the environmental triggers is essential for effective long-term management, and combining strict sun protection with professional treatments helps minimize flare-ups while giving skin a chance to recover.